There have been major advances in the treatment of diabetic retinopathy over the last decade. There are now different methods to treat it and we have become more successful in improving the vision of patient’s who suffer with this serious condition. Each patient will be assessed carefully and advised of the best management approach. We discuss each treatment’s benefit and possible side effects so the patient is fully aware of our goals prior to commencing treatment.
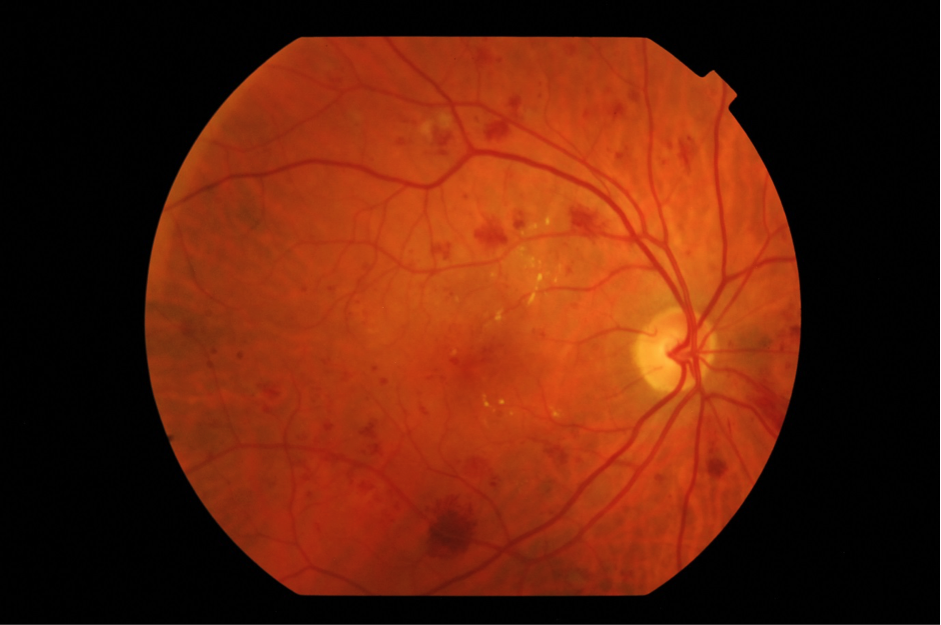
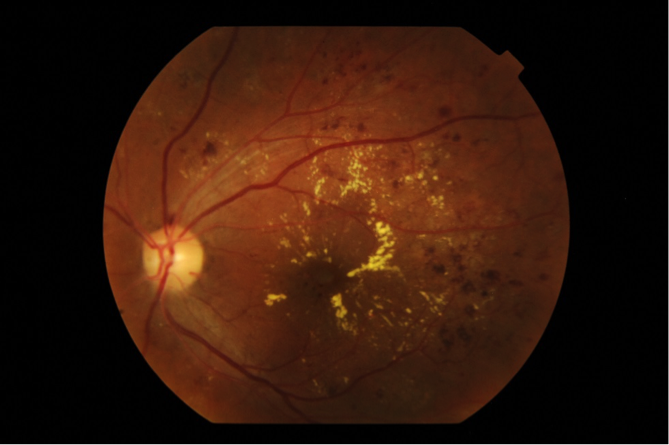
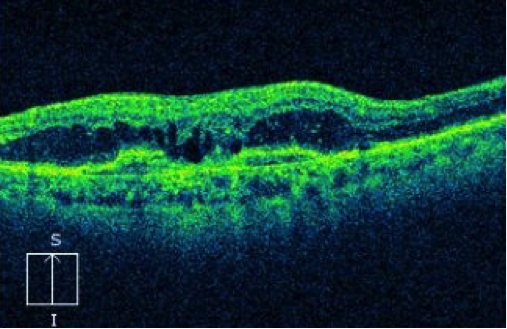
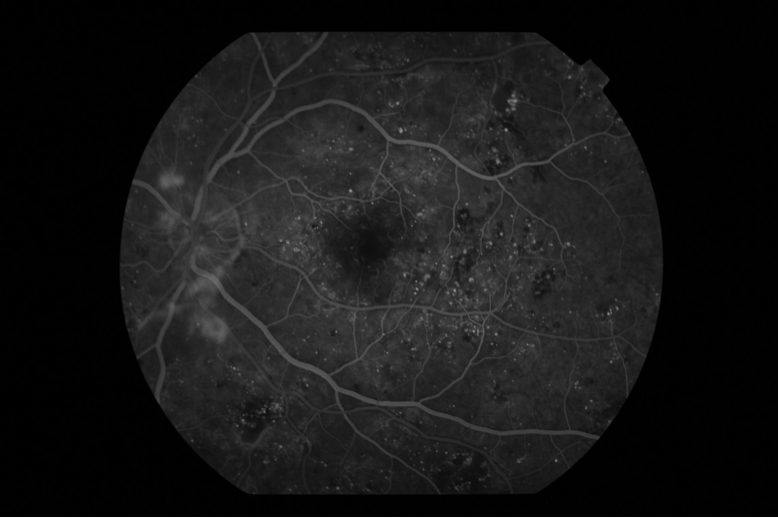
This is now the main approach to treat swelling of the retina (diabetic macular oedema). It involves injection of drugs into the eye cavity (vitreous). These drugs include Avastin, Lucentis and Eylea. They work by blocking the effect of the chemical produced in the eye with diabetic retinopathy called VEGF (vascular endothelial growth factor).This chemical is the cause of blood vessel leakage in macular oedema and the development of new retinal vessels in proliferative diabetic retinopathy.
Anti –VEGF injections are performed at the Norther Eye Centre without having to be admitted to hospital. They are done under local anaesthesia with no pain felt. We have special expertise in treating diabetic retinopathy and stream line your visit efficiently.
Anti VEGF injections need to be repeated regularly every few weeks to stabilise the macula and prevent recurrent vessel leakage
In some cases steroid drugs may be used to treat swelling of the macula (macular oedema). They can be in the form of a suspension or an implant that releases small doses of steroid over a few months. Repeated injections may also be necessary.
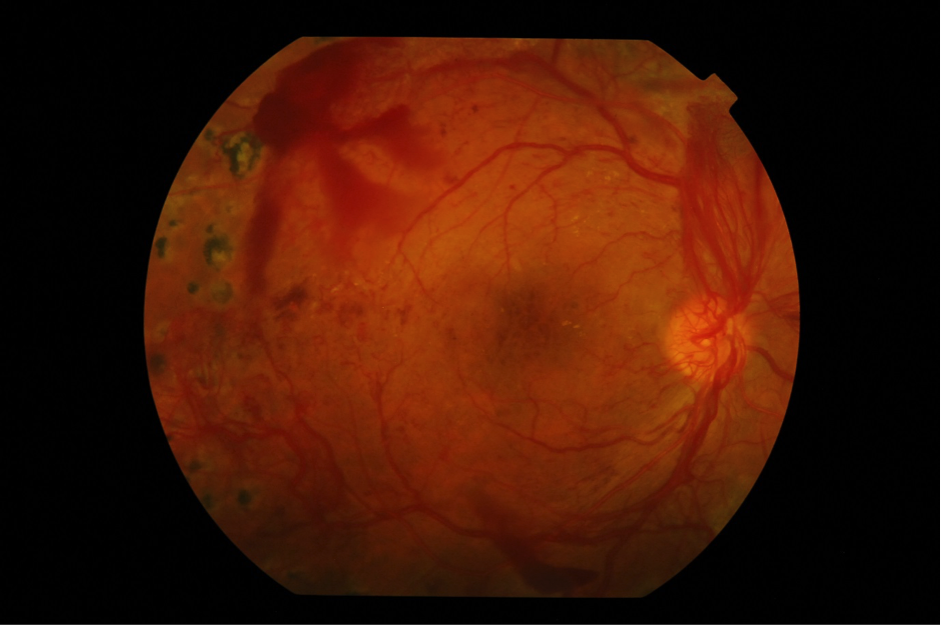
Thermal laser has been used to treat diabetic retinopathy for many decades. It is the main treatment for advanced stage proliferative diabetic retinopathy. Laser treatment is available at our centre and is applied promptly to the patient whilst sitting under anaesthetic eye drops. Some patient may require anaesthetic injection if they feel pain. The treatment is applied over 2 to 3 sessions.
Laser may also be used as an added treatment for swelling of the macula (diabetic macular oedema) usually after a course of anti-VEGF injections.
Surgery may be necessary for some patients with diabetic retinopathy including those with un-resolving vitreous haemorrhage or with diabetic tractional retinal detachment. The surgery is performed at a day surgery centre in Melbourne which has the latest surgical equipment. Dr Saf Bassili is a highly trained vitreoretinal surgeon with many years of experience.